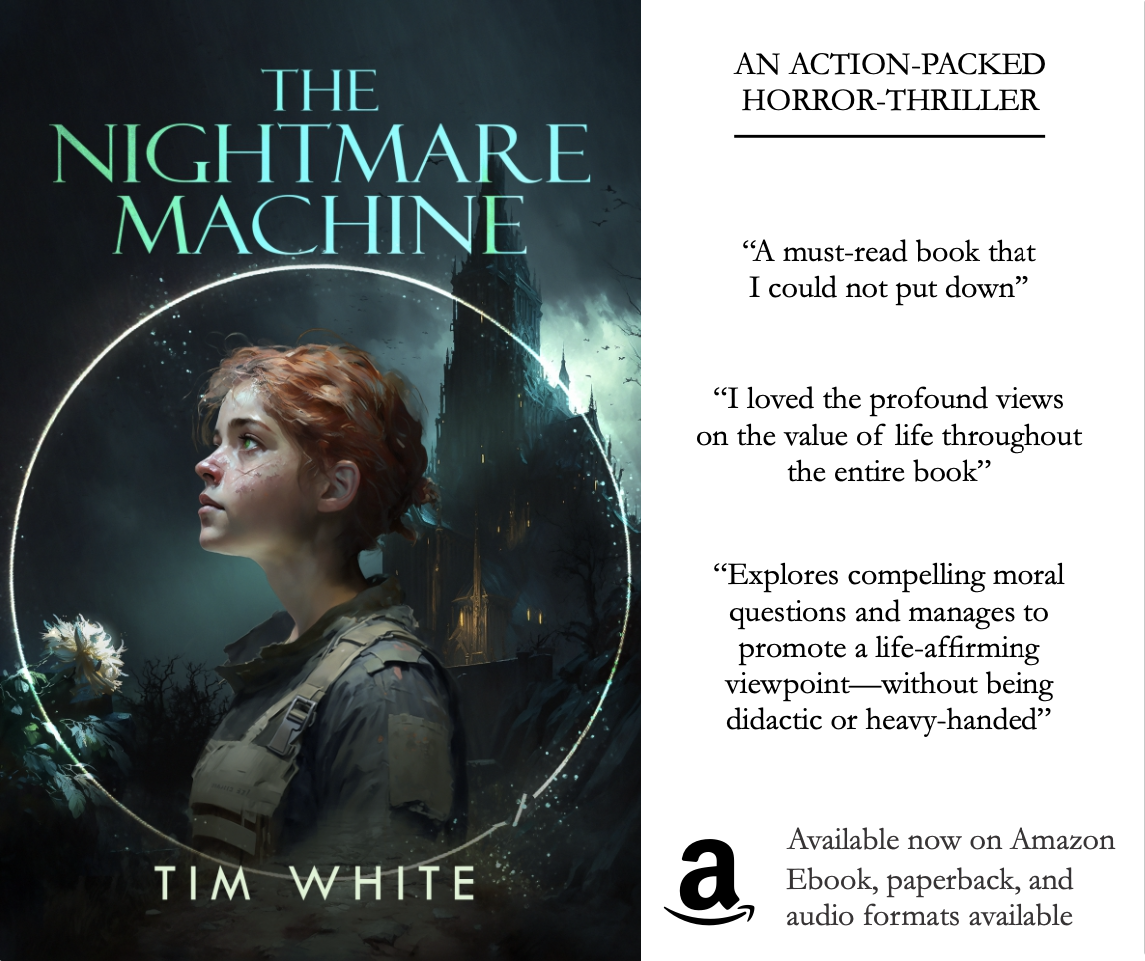
This article is dedicated to Anna Tomalis, a young girl who died of liver cancer on August 15, 2008. Anna’s parents desperately sought experimental treatment that might have saved her life, but were delayed for months by FDA bureaucracy. Anna finally received approval to obtain treatment through a clinical trial in July, but died after receiving just one round of treatment. She was thirteen years old.
Abigail Burroughs was not the typical cancer patient: She was just nineteen years old when she was diagnosed with squamous cell cancer that had spread to her neck and lungs. Her prognosis was poor, but a then-experimental drug, Erbitux, offered the hope of saving her life.
Abigail was denied that hope by the Food and Drug Administration. Because the drug was considered experimental, she could receive it only as part of a clinical trial—and Abigail was ineligible to participate in any trials at the time. Despite the best efforts of her family, friends, and doctor, Abigail was unable to receive the treatment that might have saved her life. At twenty-one years old, Abigail died of her disease.1
Abigail’s father, Frank Burroughs, thought other patients with life-threatening illnesses should not be denied the ability to try any treatment that might give them a chance. In his daughter’s name, he formed the Abigail Alliance for Better Access to Developmental Drugs, which sued the FDA in 2003. The group argued that the FDA’s restrictions on access to experimental treatments constitute a violation of the right to self-defense as well as of the Fifth Amendment right not to be deprived of life, liberty, or property without due process of law. In August 2007, the Appeals Court of the District of Columbia struck a blow against the Abigail Alliance, and against individual rights, when it ruled that patients, even the terminally ill, do not have the right to receive treatment that has not been approved by the FDA.2
Erbitux has since been approved by the FDA to treat cancer of the head and neck—too late, of course, for Abigail Burroughs. How has America come to a point where the government denies dying patients the right to try to save their own lives? To answer that question, let us begin with a brief history of the Food and Drug Administration.
A Brief History of the FDA
Prior to the 20th century, the government did not regulate pharmaceutical products in the United States. Although Congress had considered federal regulations on food and drug safety as early as 1879, it had refrained from passing any legislation in this regard. However, with the muckraking journalism of the early 1900s, and especially with the publication of Upton Sinclair’s novel The Jungle, which portrayed unsavory practices in the meatpacking industry, the American public clamored for laws to ensure the safe production of food and drugs. This public outcry pushed Congress to pass federal legislation in 1906. As the resulting Food and Drugs Act applied to drugs specifically, products were required to be sold only at certain levels of purity, strength, and quality; and ingredients considered dangerous (such as morphine or alcohol) had to be listed on the product’s label. Violators would be subject to seizure of goods, fines, or imprisonment. Thus, in order to enforce the Act, the Food and Drug Administration was born.3
In its early years, the agency focused primarily on food rather than on pharmaceuticals, but in 1937 it increased its focus on drugs after a new formulation of sulfanilamide, a drug that had previously been successfully used to treat certain bacterial infections, proved to be deadly. The drug’s manufacturer, S. E. Massengill Company, had dissolved an effective drug in a toxic solvent. More than one hundred people, babies and children among them, died as a result of taking Massengill’s product, known as Elixir Sulfanilamide.
Under the 1906 Food and Drugs Act, the FDA was not authorized to prosecute Massengill for selling an unsafe drug, and the agency had the power to recall Elixir Sulfanilamide only via a technicality. Because “elixir” was defined as a drug dissolved in alcohol, and because Massengill’s formulation used the nonalcoholic solvent ethylene glycol, the product was technically mislabeled, bringing it under FDA jurisdiction and enabling the agency to recall the product. The public and legislators wanted more: They wanted the FDA not only to recall mislabeled products, but to prevent the sale of unsafe drugs in the first place. Thus, popular demand gave rise to the Food, Drug, and Cosmetics Act of 1938, which greatly expanded the FDA’s authority.4
The most important change brought about by this Act was a shift in the burden of proof. Rather than prosecuting a drugmaker after the fact for having fraudulently marketed a product, the FDA would now require proof of safety before a drug could be marketed at all.5 (Note that this required manufacturers to prove a negative—i.e., that a given drug would not harm consumers.)
After World War II, pharmaceutical companies came under still more scrutiny. Then, as now, complaints about the cost of drugs reached Congress, and in 1961 Senator Estes Kefauver led the charge in an investigation not only of drug pricing, but of the relationship between the drug industry and the FDA. Kefauver sought to pass legislation that would increase the agency’s authority over drug production, distribution, and advertising. Whereas previously proof of safety alone was required to gain FDA approval, the proposed law would require drug manufacturers also to prove the efficacy of their products.
Kefauver’s bill might have languished in congressional debate but for the emergence at that time of data showing that thalidomide, which was then sold as a sleep aid and antinausea medication for pregnant women, caused severe birth defects in the children of women who took it. Thalidomide had not yet been approved for use in the United States at that time due to concerns of an FDA reviewer over a different side effect noted in the drug’s application for approval. The drug was widely used in other countries, however, and the babies of many women who used it were born with grotesquely deformed limbs. As their harrowing images flooded the media, Americans realized they had narrowly escaped inflicting these deformities on their own children. The resulting public outcry led to Kefauver’s bill being made law in 1962. This law served as the cornerstone for the wide powers that the FDA acquired thereafter, from requiring companies to include warnings in drug advertisements to dictating the way companies must investigate their own experimental compounds.6
Thus, although the scope and power of the FDA were modest at the agency’s inception, its scope widened and its power increased markedly in the decades that followed. Now, a century later, the agency’s purview includes foods and drugs for humans and animals, cosmetics, medical devices (including everything from breast implants to powered wheelchairs), blood and tissues, vaccines, and any products deemed to be radiation emitters (including cell phones and lasers). And the agency’s power is nothing short of enormous. Let us consider how the agency wields this power, specifically in regard to drugs.
The FDA’s Drug Dealings
The FDA is charged with approving all drugs before they can be sold in the United States. A company seeking FDA approval for a drug must present the agency with data showing the drug’s safety and efficacy, usually including trials in animals and always including trials in humans, the latter of which require FDA approval before they can begin. The company then compiles these data and presents them to the Center for Drug Evaluation and Research (CDER), a subdivision of the FDA, in the form of a New Drug Application, or NDA. (The NDA involves an enormous amount of paperwork for a pharmaceutical company: an estimated two hundred thousand unique pages of data, which must then be submitted in triplicate. Drug manufacturers often must hire trucks to transport the forms to FDA headquarters.)7 CDER then reviews the data and decides not only whether the drug will be approved for sale, but also which diseases it may be used to treat, which patients may take it, the permissible dosage, the permissible frequency, what claims may be made about the drug, and what warnings it must carry about the drug’s side effects. This process is known as the development of the drug’s “label.” Once a drug’s label is developed, if the drugmaker seeks FDA approval for new uses, it must submit additional data and pay additional review fees.
If a drug is approved, the FDA continues to monitor both it and the manufacturer. The FDA conducts periodic inspections of manufacturing facilities (both foreign and domestic) to ensure that drugs are being produced according to the agency’s standards. If the FDA discovers violations, it can issue penalties ranging from fines, to seizure or recall of products, to criminal prosecution. Further, the FDA collects reports of side effects from pharmaceutical companies and from patients to determine whether to issue warnings about such effects.
The FDA also regulates advertising and promotional materials used to market drugs, ensuring that drug companies market their products only for their approved uses, and that the companies neither overstate the benefits of a drug nor understate its hazards. The agency mandates that drugmakers include “appropriate fair balance,” or statements about a drug’s safety risks, in all materials that make claims about a drug. (For some products deemed particularly risky by the FDA, merely mentioning the brand name of the product in an ad, without making any claims as to its efficacy or safety, is enough to require that “appropriate fair balance” statements be made.)
Pharmaceutical companies are required to submit copies of all promotional materials, whether aimed at physicians or consumers, to the FDA for the agency’s records. If the FDA deems materials to be in violation of its standards, the agency may issue warning letters demanding corrective actions, such as destruction of the offending materials and public retraction of the offending statements. If the company fails to respond in a manner acceptable to the FDA, the agency may seize the offending materials or seek an injunction against the company.
Thus, the FDA of 2008 is almost unrecognizably different from the FDA of 1906. Whereas the FDA of yore was limited to reactively punishing companies that violated the agency’s relatively few standards, today’s FDA proactively prevents companies from selling drugs until the agency has reviewed truckloads of data and is satisfied as to the drugs’ safety and efficacy; inspects manufacturing facilities to see that the agency’s standards are being met; and regulates and monitors the content of drugmakers’ advertising and promotional materials. These functions require a staff of nearly eight thousand employees and an annual budget of $2.4 billion.8
The Impracticality of the FDA
Few would oppose the goal of safe, effective drugs. But is the FDA really helping to accomplish that end? It is not. In fact, in its efforts to protect patients’ safety, the FDA has unwittingly prolonged the suffering and hastened the deaths of countless Americans. Abigail Burroughs, who died waiting for a treatment that the FDA later approved for her condition, is unfortunately one of a tragic many.
FDA requirements that drugmakers prove both safety and efficacy of a drug before marketing it mean that the companies must put a given experimental compound through multiple rounds of laboratory, animal, and clinical trials before it can be sold to the public. These trials can take many years—not to mention the time it takes the FDA to review the data generated from the trials. From the time a molecule is discovered in the laboratory to the day that molecule can be sold to Americans as an FDA-approved drug takes an average of eleven years.9 In the meantime, patients such as Abigail who might benefit from an unapproved drug are forbidden to receive it (unless they are fortunate enough to be able to participate in a clinical trial). Consequently, many suffer needlessly and die prematurely. As John Stossel writes:
Some years ago, the FDA held a news conference and proudly announced, “This new heart drug we’re approving will save fourteen thousand American lives a year!” No one stood up at the press conference to ask, “Excuse me, doesn’t this mean you killed fourteen thousand people last year—by delaying its approval?” No one asked that because reporters don’t think that way, but that’s what the FDA’s announcement meant. If the drug saves 14,000 lives a year, then 14,000 people died each year while the drug awaited approval.10
And because the people who die while waiting for the FDA to approve drugs that could save their lives are not counted as deaths caused by the FDA-mandated delay, FDA officials actually have an incentive to delay the approval of drugs. Although the media never mention the thousands who suffer or die while waiting for a drug to be approved, they are quick and loud in their reporting of side effects or deaths attributed to any drug that the FDA has approved—and to blame the agency for not being cautious enough. “The FDA catches all sorts of grief for its decisions that let drugs on the market,” observes Richard Epstein. “The tendency in all cases is to have a bureaucratic incentive to avoid the heat.”11
The devastating slowness with which the FDA approves lifesaving therapies is exemplified in the story of the cancer treatment Avastin. Although Avastin has been on the market since 2004, it was initially approved only to treat a narrow range of patients: those with colon or rectal cancer that had spread to other parts of the body. In 2005, data were presented at two large meetings for cancer specialists showing that Avastin also slowed the growth of tumors in patients with late-stage breast cancer. Yet it was not until February 2008—more than two years after the initial presentation of the data—that the FDA approved Avastin for that use. More than forty thousand American women die of breast cancer each year,12 meaning that, in the time the FDA took to approve Avastin for that use, scores of thousands of women who might have benefited from the drug by living longer, less-painful lives instead suffered more and died sooner.
Given the delay between an announcement of positive results for a drug and the FDA’s actual approval of that drug, physicians often prescribe a drug for uses for which it is not approved (so-called “off-label use”). This is both legal and commonplace (20 percent of prescriptions are for off-label uses).13 But this practice does not eliminate the problem. Although a physician would have been able to prescribe Avastin for breast cancer in 2006, lack of FDA approval for that use meant that few insurance companies would have covered the drug for that use.
Patients such as Abigail Burroughs who need a drug that has not yet been approved by the FDA for any use have no recourse but a clinical trial or so-called “compassionate use.” Clinical trials require a substantial commitment on the part of the patient that may include more frequent checkups and medical tests than he would otherwise need or want, filling out mandatory questionnaires that ask for information he might not want to share, or traveling great distances to a center where the appropriate trial is being conducted. All this assumes the patient is even eligible to enter the trial: The design of every clinical study contains inclusion and exclusion requirements (which may be dictated by the FDA) that render many patients ineligible to participate in the study. Thus, a patient who wants to try a new treatment for his condition is likely to be denied that treatment by the FDA. Likewise, applying for “compassionate use”—a program in which the FDA reviews patients’ requests to receive experimental treatments on a case-by-case basis—involves much paperwork and time on the part of the patient, and there is no guarantee that the FDA will approve the request.
The discussion thus far has focused on drugs that eventually do obtain FDA approval and are thus eventually able to help patients. Countless drugs enter the FDA’s approval process but are rejected; others are abandoned by their manufacturers based on forecasts that approval is unlikely. Many of these drugs could help countless people if those people were able to receive them.
The FDA does not reject only those drugs that it concludes cannot help anyone. The FDA’s decisions are made based on the average performance of a drug over the entire sample of patients in one or more clinical trials. This process leads to the rejection of drugs that might not work on the majority of the population but that could alleviate the suffering and save the lives of many. As Richard Epstein explains:
Suppose that we rate patient response to treatment on an (admittedly arbitrary) scale of 0 to 100, where the current drug has a mean average of 50 but a variation in responses from 25 to 75. Now put a new drug on the market that has a mean average of 45, with a variance of 20 to 70. The question is whether the second drug should be allowed on the market, when each relevant parameter is 5 points below that of the original drug. . . . [A]ny person who scores X with the current drug will turn X minus 5 with the new one. Individual choice could only compound error. But heterogeneity totally undermines that assumption. Now even though the whole curve has shifted to the left for the new drug, some fraction of individuals will score better with the new one than the old one. Since we don’t know who these individuals are, we pay a high price in letting the entire patient population have only one choice instead of two.14
In short, if a drug is inexplicably effective in a subset of the test population but appears to be ineffective across the larger test group, the FDA will not approve it—even though many patients might benefit by taking the drug. The FDA’s decisions are based on collective results—to the detriment of countless actual individuals.
In addition to keeping drugs away from suffering and dying people who need them, the FDA also causes a huge increase in costs for pharmaceutical companies—an increase they pass on to Americans in the form of higher drug prices. The cost of developing a drug, from the time a molecule is discovered in the laboratory through animal trials and multiple stages of trials with human subjects, is estimated at $800 million.15 Note that the time during which the drug is protected by patent law includes those years during which the drug is in development but cannot be sold because FDA regulations forbid marketing the drug without approval. Thus drugmakers have far fewer years than other inventors to profit from their discoveries. Yet they have a massive monetary cost to distribute over those fewer years, knowing that their products are easy to copy once patent protection is lost.16 Given that patent protection is typically granted for twenty years,17 and given that eleven of those years are lost waiting for FDA approval, is it any wonder that patients and politicians alike are crying out about the high cost of drugs?
And the price Americans pay for FDA regulations is far greater than the higher prices paid for prescriptions at the pharmacy. The uncounted costs of unnecessary suffering and earlier-than-necessary death are consequences not only of unapproved drugs and high-priced prescriptions, but also of the unseen stifling of innovation.
With an $800 million investment required to bring a drug from molecule to marketplace, small companies simply do not have the resources to complete the process, and larger ones are unwilling to spend so much money on a drug with less-than-ideal prospects. Which is a surer way to make money in the current regulatory environment: taking an $800 million gamble developing a new drug that might treat a previously untreatable disease—but that might not be approved by the FDA—or avoiding such risk and instead making a small manipulation to an existing blockbuster drug and then marketing it with a fresh face among the other highly profitable drugs that treat the same previously treatable ailments?
This is why one does not read in the news today about a new discovery on the order of penicillin, which cured a host of diseases that were previously untreatable. (In fact, it is quite likely that if drugs such as penicillin or aspirin—mainstays of medicine—were discovered today instead of a century ago, they would not survive the FDA approval process.)18 Instead, one sees a panoply of cholesterol medications (several of which are merely combinations of previously existing drugs), sleep aids, and antidepressants. Without the huge costs and risks of drug development imposed by the FDA, how much more time, money, and brain power would the pharmaceutical industry be putting toward research and development of new drugs? We may never know, but what we do know is that, as the New York Times observed in 2002: “The industry’s output of new drugs has risen only modestly in the last two decades despite a more than sixfold increase, after adjusting for inflation, in research and development spending, to more than $30 billion annually. In the last few years, the output has actually declined.”19
Given what the FDA costs America—in the human suffering and lives lost while patients wait for drugs to be approved (or not approved), in the higher drug prices resulting from regulation, and in the life-enhancing therapies that go unproduced because the cost of developing them is too high—one might suppose that the FDA must have some redeeming value that justifies its existence. One might suppose that at least the drugs that do receive FDA approval are safe and thus that Americans are in some way benefiting from this agency. One might suppose this, but one would be wrong.
Consider Vioxx, the anti-inflammatory drug famously pulled from the market in September 2004 when results from a clinical trial indicated that patients taking Vioxx had a higher rate of cardiovascular problems than patients taking placebo. Although this observation is not enough to establish a causal relationship between Vioxx and heart disease, it alarmed the public and regulatory officials enough that Merck, the manufacturer of Vioxx, “voluntarily” (under intense political pressure) withdrew the drug from the market and continues to be plagued by Vioxx-related lawsuits. The FDA approval process, as long and arduous as it is, wasinsufficient to discover the safety problems attributed to Vioxx. Similar issues have arisen with the diabetes drug Avandia and the birth control patch Ortho Evra. Likewise, in the case of heparin, an anti-clotting drug that has been widely used for more than fifty years,20 the FDA failed to prevent contaminated product from reaching consumers. The result was at least sixty-two deaths between January 2007 and March 2008.21
One might object that this criticism is unfair on the grounds that in the absence of the FDA these drugmakers would just have taken these drugs straight to market. But this objection overlooks the fact that because the FDA exists and is officially charged with ensuring the safety of all drugs sold in America, the American people expect and rely on the agency to do just that. If the FDA did not exist, the marketplace would demand the drug-monitoring equivalent of Underwriters Laboratories (UL) in electronics or A.M. Best in insurance—and such private companies would do the job far better than the FDA does (more on this later).
In sum, the FDA’s policies keep countless patients from receiving countless lifesaving and life-enhancing medications from pharmaceutical companies who are willing either to sell those medications or to give them away as part of a clinical trial; they drive up the cost of producing drugs and thus the price of drugs at the pharmacy; they stifle the development of new and innovative therapies; they create a false sense of security; and they keep profit-driven businessmen from developing free-market means of providing better guarantees of drug safety and efficacy.
That is a brief indication of how the FDA hinders health. Let us turn now to the related and more fundamental matter of how it violates rights.
The Immorality of the FDA
Although the FDA’s stated purpose is to safeguard the health of Americans from the risks of unproven medicines, its actual function is to violate the rights of businessmen and customers to trade with each other by voluntary consent to mutual benefit.
The FDA forcibly prohibits drug manufacturers from creating, testing, and marketing their own drugs according to their own best judgment. Manufacturers must get permission and approval from the FDA all along the way, and if that permission or approval is withheld, the drug-making, drug-testing, and drug-marketing process necessarily comes to a halt, for the FDA’s demands are backed by government force: the threat of seizure of products, of enormous fines, of the closing of a company’s doors.
Likewise, the FDA forcibly prohibits customers who wish to contract with the aforementioned businessmen from doing business with them. Abigail Burroughs was prevented by the FDA from purchasing the drugs she wanted and needed—drugs that likely would have improved and extended her life.
Because neither the pharmaceutical company nor the patient is infringing anyone’s rights by producing or selling or purchasing a drug—even a highly risky or clinically unproven drug—the FDA is violating their rights by forbidding them from contracting with each other as they see fit. In the name of ensuring safe medication in America, the FDA violates the rights of Americans to market or receive medications that could save American lives.
Another aspect of the rights-violating nature of the FDA pertains to the right to be considered legally innocent until proven guilty—a right the FDA routinely violates by forcing pharmaceutical companies to prove the efficacy and safety of their products before they may be sold. In a court of law, the burden of proof is, as it logically must be, on the prosecution to show that the defendant has committed the offense of which he is accused—not on the defense to prove that he has not committed the offense. The presumption of innocence is one of the pillars of the American justice system; it is a crucial safeguard preventing the government from using its powers against citizens on mere suspicion of guilt. Even a common criminal has this legal right—but, under FDA regulations, pharmaceutical companies and patients do not.
The FDA casts the principle of presumed innocence aside and treats drugmakers as guilty until proven innocent. Instead of prosecuting drugmakers for negligence or false advertising (or the like) after the fact, by presenting evidence of their guilt, the FDA assumes preemptively that their products are unsafe or ineffective, and that their advertising is deceptive, until the drugmakers gather data and fill out paperwork to prove otherwise. This puts the drugmakers in the impossible position of having to prove that they have not done something wrong when no evidence has been presented to indicate that they have done something wrong.
In addition to presuming pharmaceutical companies to be guilty until proven innocent, the FDA presumes patients to be irresponsible and incapable of acting rationally or in accordance with their doctor’s advice. Consider, for example, the regulations surrounding the acne medicine isotretinoin, best known as Accutane. Because the use of Accutane can cause severe birth defects, it should not be taken by pregnant women. The FDA, seeking to prevent Accutane-related birth defects, considers the advice and prescription of a doctor insufficient to prevent pregnant women from using the drug. So the agency has developed a mandatory program, iPLEDGE, for all women who take Accutane who are defined by the agency as being of childbearing potential. In order to receive Accutane, a woman must use two forms of birth control, visit her doctor every month for FDA-mandated in-office pregnancy testing, and complete a monthly quiz about her contraception use. Failure to complete any of these requirements is grounds for denial of an Accutane prescription.22 (And to ensure that doctors monitor their patients as the program requires, the FDA has made it illegal to prescribe more than one month’s supply of Accutane at a time.) The FDA has imposed a similar program for women using thalidomide, which recently re-emerged in the medical world as a treatment for certain forms of cancer—even though the vast majority of women with cancer are well beyond their childbearing years and are therefore in no danger of becoming pregnant.
Patients, like pharmaceutical companies, are treated by the FDA as guilty of some wrongdoing in the absence of any evidence to that effect. Unfortunately—and predictably—in the case of Accutane, the result of this policy is that women who want to treat their acne but are unwilling to deal with the hassle imposed by the FDA often turn to foreign Internet pharmacies, many of which get their drugs from questionable sources. The “Accutane” women get this way may be contaminated or even counterfeit23—and the women who take it are far less safe than they would be if the FDA were not regulating Accutane at all, in which case they could purchase it at the corner drugstore. This is just one of the many ways in which, by violating individuals’ rights to purchase drugs freely, the FDA actually encourages dangerous behavior.
Given the FDA’s presumption that pharmaceutical companies are guilty until proven innocent, it is no surprise that the agency severely restricts their freedom of speech. Drugmakers are prohibited not only from making fraudulent claims (as, of course, they should be); they are prohibited also from making certain truthful statements, and they are forced to spend a substantial portion of their advertising budgets denigrating their own products.
The prohibition on truthful statements pertains to so-called “off-label” promotion: If the FDA has not approved a product for use in a particular condition and thus does not include that condition in the product’s labeling, then neither the company’s sales representatives nor its advertisements may mention that condition—even if scientific evidence shows that the product treats the condition effectively. (At the time of this writing, a sales representative is not permitted even to give doctors peer-reviewed journal articles, even those written by authors with no affiliation with the company, if the articles discuss off-label use.)24 This means that a doctor seeking information on the latest uses of a drug often cannot get that information from what is likely the most complete and reliable source of knowledge on the subject—the drug’s manufacturer. If a doctor asks unsolicited questions about unapproved uses of a drug, then and only then may certain employees—but not sales representatives—of the drugmaker provide him with some information. But this information, too, is severely restricted.
The way in which the FDA forces drugmakers to denigrate their own products using their own budgets pertains to the nebulous requirement that all of a drug’s promotional materials contain “appropriate fair balance.” This mandate means that whenever a drugmaker issues claims about the efficacy of a drug, it must also include “appropriate fair balance” statements about the drug’s safety risks. Because the phrase “appropriate fair balance” is not and cannot be objectively defined, drugmakers have no way of knowing whether their advertisements contain sufficient qualifiers. Thus, out of concern that the FDA might issue a warning letter (which is a matter of public record and thus can become a trigger for lawsuits), companies frequently err on the side of caution, fearfully abstaining from making positive claims that their drugs work and anxiously informing potential customers of all the side effects that “could” happen, even if the drug is effective in almost all patients whereas the side effects occur in only a tiny fraction of patients. As Richard Epstein puts it, “Quite simply, any marketing campaign that mirrors the FDA assessment will not be fair and accurate, but unduly pessimistic.”25 The next time you hear a drug advertisement on television or the radio, observe the amount of time the narrator spends enumerating the drug’s side effects. In some cases, a narrator will even issue warnings concerning matters that are obviously unrelated to any legitimate expectation regarding the purpose or efficacy of the drug—such as when an ad for a drug that treats erectile dysfunction includes warnings to the effect that the drug does not protect against sexually transmitted diseases.
The FDA’s violations of drugmakers’ right to freedom of speech lead directly to increased costs for drugmakers. In order to convey information about new uses for their drugs, companies must spend millions of dollars and thousands of man-hours first conducting additional clinical research and then filing reams of paperwork with the FDA, which then takes months (or more, as was the case with Avastin) to review the application. These costs, of course, are passed on to consumers, as are the costs of hiring staffs of doctors, lawyers, and regulatory specialists whose sole purpose is to review company materials to ensure that they will pass the FDA’s non-objective scrutiny.
The FDA violates the rights of both pharmaceutical companies and patients by forcing them to act against their own best judgment regarding the production and consumption of medicines. A pharmaceutical company, having tested a drug in its laboratories, having obtained the informed opinion of experienced scientists, and having deemed a drug ready for the market, may not act on that judgment. Instead, it must submit to the decisions of FDA bureaucrats who may never have produced a useful molecule in their lives. A company whose researchers have found a new use for a drug that could enhance the lives of millions of Americans is not free to communicate this fact to doctors quickly and thus allow patients to benefit from the new knowledge as soon as possible. Instead, it must wait until the FDA sees fit to acknowledge the information—if it ever does. And a patient who is willing to risk unknown side effects from a new drug because he knows his illness will kill him if he does nothing, is forbidden to act on his judgment. Instead, he is told that the risk is too high—which means: “We at the FDA would rather let you die than let you take this drug that might save your life.”
Thus, the FDA says to pharmaceutical companies: Don’t decide for yourselves whether your product is good or worthy of marketing to Americans; don’t decide which facts are important to communicate to the public; don’t decide which tests are sufficient or when your drug is ready to be sold—we will decide all this for you. To patients, the agency says: Don’t consider your own values or your personal context and decide which risks are worth taking or whether your life is worth any risks at all; don’t think that consulting your doctor and doing your own research regarding your condition is sufficient to make an informed decision—we will decide all this for you.
The FDA violates one’s right to act on one’s own best judgment—which means that it violates one’s right to life. If you think this is an exaggeration, ask Abigail Burroughs’ parents; they will confirm its accuracy.
When a person or an organization outside of government violates an individual’s right to life, we properly identify him or it as immoral and treat him or it accordingly. It is high time we applied that same standard to the FDA. The agency is immoral. It has no moral right to exist. It should be abolished.
A Vision of America Without the FDA
The abolition of the FDA would not mean, as some suggest, that pharmaceutical companies would turn into snake-oil salesmen peddling false “cures” to a gullible public. Rather, it would mean that a marketplace full of profit-seeking businessmen and industrialists would be free to innovate with respect to the best ways to ensure the efficacy and safety of drugs. A free market would still involve risks; risk is inherent in human life, and nothing can change that. But the profit motive, businessmen’s reputations, stockholders’ demands, insurance companies’ requirements, the judgment of doctors and patients, laws against fraud, private review organizations, and other free-market factors would contribute to the establishment and maintenance of a market in which the safety and efficacy of drugs would be at the peak of what current technology and market demand would bear.
Although critics of free markets will rush to say that profit-seeking drug companies will lie about their products in order to make money, the fact is that the greatest protection from harmful products is a manufacturer’s desire to make a profit. No business can last long if its product provides poor value for the price or harms the people who buy it. The long-term best interest of a company and its profit-seeking shareholders is not served by foisting an inferior product on consumers, because the truth will eventually come out. To succeed and make money in a free market, drugmakers, like producers of any other goods or services, must convince a discriminating public of the worthiness of their product. As John Stossel puts it:
[W]ithout the FDA, how would doctors and patients know which drugs were safe and effective? The same way we know which computers and restaurants are good—through newspapers, magazines, and word of mouth. . . . [I]n a free, open society, competition gets the information out, and letting that process flow protects consumers better than government command and control.26
If a company misleads consumers about the efficacy or safety of its products, that company’s reputation will suffer, perhaps fatally, when the truth is exposed. To make not just a quick buck, but long-term profits, pharmaceutical companies must consistently deliver drugs that work and that, when used in accordance with the manufacturer’s specifications, are safe.
If an unscrupulous manufacturer does cause harm to consumers by lying about a product’s efficacy or safety, the manufacturer has committed fraud and can be prosecuted in a court of law. Consider the Massengill Elixir Sulfanilamide case that led to the expansion of the FDA’s powers: Massengill lied to its customers by calling the product an “elixir,” which told consumers they were getting a drug dissolved in alcohol, a safe solvent in the appropriate quantity. In fact, it was not an elixir; the solvent was not alcohol, but ethylene glycol, a substance toxic at much smaller doses. Had consumers known the facts about the product, they would not have chosen to buy it—and Massengill had misrepresented the facts. Thus, the appropriate response to the situation would have been to prosecute Massengill for making fraudulent claims about its product.
How would a free market protect consumers from a company that caused harm to consumers without falsely advertising its product? For example, what if mistakes in the manufacturing process led to a contaminated batch of product, as occurred recently with the anticoagulant drug heparin? Again, no environment is risk-free; mistakes and accidents will happen in any market. But the profit motive remains the best safeguard against such errors—because the way to make money is not to poison one’s customers but to provide them with good, safe products. No drugmaker can afford to be known as the one who killed patients due to slipshod manufacturing practices. Nor can its provider of liability insurance afford to permit the drugmaker to engage in such practices; which is why insurance providers closely monitor the manufacturing process. And in the rare case that a product does cause demonstrable harm (whether by accident or through neglect), the American legal system is equipped to handle the situation.
A more complicated question is: What if a drug has side effects that are not apparent in the early stages of the drug’s development? Unlike clothing, cars, and most other consumer goods, drugs have chemical effects on the human body; such effects constitute their very usefulness. But drugs can and often do produce negative effects as well. A birth control pill might cause nausea; a cold medicine might cause drowsiness; a powerful chemotherapy drug that kills cancer cells might suppress a patient’s immune system so thoroughly that the patient then contracts a life-threatening infection. In many cases, such as with Vioxx, these safety risks are not known until the drug has been used to treat many thousands of patients over the course of years. How would an FDA-free market protect Americans from risks such as these?
As we have seen, Vioxx was sold with FDA approval for years before a possible connection with heart disease was discovered. Although a free market in medicine would not eliminate risks, it would enable patients to use their own best judgment in assessing those risks against the benefits of a drug. Patients could make these decisions with the advice of a trusted physician. Acting on one’s best judgment does not preclude the possibility of seeking expert advice. Doctors are experts in medicine; patients are experts concerning their own wishes, needs, and willingness to take risks. A patient with terminal cancer who expects to live only another six months might be more willing to try a drug with a potentially fatal side effect than a patient whose cancer is at an earlier stage and expects to have a normal life span. Only the patient can make a sound decision about what is right for him in this regard. With the aid of his doctor, a patient can make decisions that account for all the relevant and available facts. This is precisely what the FDA cannot do.
Nor in the absence of the FDA would doctors be the only resource patients have when seeking guidance about a drug’s benefits and risks. Currently, a number of private professional organizations, such as the American Society of Clinical Oncology in cancer and the American Psychiatric Association in mental illness, provide treatment guidelines based on expert evaluation of the available options. Doctors and patients can choose, but are not forced, to follow these guidelines when deciding which drugs to prescribe or take. These guidelines, unburdened by government bureaucracy, are updated far faster, and are thus more useful to patients and physicians, than FDA product approvals.
Moreover, as mentioned earlier, in the absence of the FDA, private certification agencies that could grant a meaningful “seal of approval” to drugs would be in enormous demand. Consider Underwriters Laboratories (UL), which tests electrical appliances and certifies their safety with its seal. UL is a privately owned, for-profit company; it has no coercive means of gaining customers or establishing a reputation; it is not a government agency like the FDA; yet its safety standards are so well respected that few consumers buy appliances that are not UL listed. Similarly, A.M. Best, an insurance-rating and information agency, profits by issuing in-depth reports so that consumers can determine, among other things, the financial ability of insurance companies to pay claims. In the absence of the FDA, similar ratings companies would arise to certify the efficacy and safety of drugs. Not only would these be better than the FDA because the element of coercion would be removed (consumers, if they wished, could ignore ratings when purchasing drugs if they came to a different assessment of the risks and benefits involved); such companies, unlike a government agency, would be in competition with each other to provide the most reliable, most up-to-date, most informative ratings. This competition would only enhance the amount of information available to patients and physicians when making treatment decisions.
How would doctors, patients, or ratings companies be able to judge the risks and benefits of a drug? Pharmaceutical companies today spend considerable amounts of money sponsoring so-called “post-marketing” research—that is, research on a drug after it has already been approved by the FDA. Why would a drug company bother to do even more research than is necessary to gain drug approval? In some cases, the company does so because the FDA has demanded post-marketing research as a condition of drug approval, but in most cases, these trials are sponsored simply because the company wants to know more about the drug. After all, a company needs to have evidence in order to make true claims when promoting its product, and clinical trials are one crucial way to obtain that evidence. Independent organizations, such as hospitals and nonprofit patient advocacy groups, could also conduct research if they wished to learn something new about an existing drug. As with post-marketing pharmaceutical company-sponsored research, independent research takes place even with the existence of the FDA; there is no reason to suppose that it would disappear in the agency’s absence.
Thus, abolishing the FDA would not create a vacuum in which pharmaceutical companies would rush to make exaggerated claims about their products or in which patients would have to make decisions about their health care in the absence of quality information. In fact, the media, existing fraud and tort laws, and the guidance available from doctors and private organizations would combine to create an environment in which patients could make far better-informed decisions than they are able to make under the tyranny of the FDA.
Removing FDA regulation from the pharmaceutical industry would free pharmaceutical companies to innovate; it would free doctors and patients to act on their own best judgment; it would lower the cost of health care and increase the quality and availability of medicine. In short, removing the FDA’s grip on the pharmaceutical industry, on patients, and on doctors would be the best thing since penicillin.
You might also like
Endnotes
1 Sue Kovach, “The Abigail Alliance: Motivated by Tragic Circumstances, Families Battle an Uncaring Bureaucracy,” Life Extension, September 2007, p. 26.
2 Andrew Pollack, “Court Rejects Patient Right To Use Drugs Being Tested,” New York Times, August 8, 2007. Accessed at http://query.nytimes.com/gst/fullpage.html?res=980CEEDA1230F93BA3575BC0A9619C8B63&st=cse&sq=abigail+alliance&scp=2.
3 Ira R. Berry, ed., The Pharmaceutical Regulatory Process (New York: Marcel Dekker, 2005), pp. 9–15.
4 Carol Ballentine, “Taste of Raspberries, Taste of Death: The 1937 Elixir Sulfanilamide Incident,” FDA Consumer, June 1981. Accessed at http://www.fda.gov/oc/history/elixir.html.
5 Berry, Pharmaceutical, p. 21.
6 Berry, Pharmaceutical, pp. 28–32.
[groups_can capability="access_html"]
7 Aaron Smith, “Generic Drug Flood Headed Our Way,” CNN/Money, August 3, 2005. Accessed at http://money.cnn.com/2005/08/03/news/fortune500/generic/index.htm.
8 Andrew C. von Eschenbach, Statement on Support of Science of the FDA before the House Subcommittee on Oversights and Investigations, January 29, 2008. Accessed at: http://www.hhs.gov/asl/testify/2008/01/t20080129c.html; U.S. Food and Drug Administration, “Summary of FDA’s FY 2009 Budget.” Accessed at: http://www.fda.gov/oc/factsheets/budget2009.html.
9 Andrew Pollack, “Despite Billions for Discoveries, Pipeline of Drugs Is Far From Full,” New York Times,April 19, 2002. Accessed at http://query.nytimes.com/gst/fullpage.html?res=9407E4DB153FF93AA25757C0A9649C8B63&st=cse&sq=%24800+million+drug+development&scp=3.
10 John Stossel, Give Me a Break: How I Exposed Hucksters, Cheats, and Scam Artists and Became the Scourge of the Liberal Media . . . (New York: HarperCollins, 2004), pp. 44–45.
11 Richard A. Epstein, Overdose: How Excessive Government Regulation Stifles Pharmaceutical Innovation (New Haven: Yale University Press, 2006), p. 117. “Tendency” reads “tendencies” in the original.
12 Ahmedin Jemal et al., “Cancer Statistics, 2008,” CA: A Cancer Journal for Clinicians, vol. 58, no. 2, March–April 2008, p. 76.
13 Stephanie Saul, “F.D.A. Plan on Medical Articles Takes More Heat,” New York Times, April 19, 2008. Accessed at http://www.nytimes.com/2008/04/19/business/19ghost.html?_r=1&oref=slogin.
14 Epstein, Overdose, pp. 121–2.
15 Pollack, “Billions.”
16 Aaron S. Kesselheim, “Intellectual Property Policy in the Pharmaceutical Sciences: The Effect of Inappropriate Patents and Market Exclusivity Extensions on the Health Care System,” The AAPS Journal, vol. 9, no. 3, pp. E306 and E309.
17 Matthew Herper, “Are Drug Patents Too Short?” Forbes,March 9, 2005. Accessed at http://www.forbes.com/sciencesandmedicine/2005/03/09/cx_mh_0309plavix.html.
18 Derek Lowe, “Aspirin: Not Approvable,” Medical Progress Today, November 17, 2005. Accessed at http://www.medicalprogresstoday.com/spotlight/spotlight_indarchive.php?id=1039.
19 Pollack, “Billions.”
20 Ehud Arbit et al., “Oral Heparin: Status Review,” Thrombosis Journal,vol. 4, no. 6, p. 1.
21 Elizabeth Weise and Julie Schmit, “Deaths Linked to Heparin Triple to 62,” USA Today,April 9, 2008. Accessed at http://www.usatoday.com/money/industries/health/2008-04-08-fda-heparin-deaths_N.htm?csp=34.
22 The iPLEDGE Program Patient Introductory Brochure, pp. 3–5.
23 Rebecca Webber, “Would You Risk Your Health for Clear Skin?” Glamour, September 2007. Accessed at http://www.glamour.com/fashionbeauty/articles/2007/08/accutane.
24 Saul, “Heat.”
25 Epstein, Overdose, p. 155.
26 Stossel, Break, pp. 45–46.
[/groups_can]